THE IMPORTANCE OF EXPOSING FALSIFICATIONS IN MEDICAL RECORDS
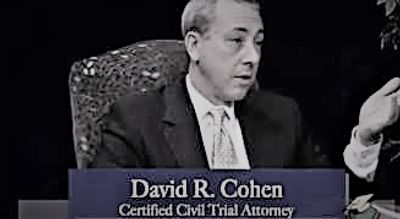
THE SUBTLETIES OF FALSIFIED ENTRIES IN THE NURSING HOME CHART (click on photo to watch video):
Over the last 19 years of my 28 year practice as a nursing home abuse attorney, it has become quite apparent that one of the most overlooked and yet important players in exposing nursing home abuse in the nursing home industry is the MDS (Minimum Data Set) Coordinator. All money that flows into a nursing home ostensibly flows through their office. Of paramount importance in this regard is the confluence of records contained in the MDS relative to the resident's ADL status and the ADL flow sheets themselves. Nursing homes are the subject of competing incentivization, depending upon which aspect of the chart is used. In the first instance, they are incentivized to paint a picture of their home as having clients who are capable of performing ADLs to a high level, and thus in little need of care. At the same time, these same they are incentivized to characterize the very same residents as being in need of a much higher level of services and capable of benefiting from such services - in order to establish a higher RUG rate (resource utilization group).
ADL flow sheets typically are not provided at the time of a chart request. However, the most efficient way to obtain them is not to ask for them until after some depositions are taken. Once it is confirmed not only that ADL flow sheets are retained, but that they are also integral components of the resident's chart, the facility is in a position that they cannot claim that they simply destroyed them, as this would be destruction of the chart in violation of OBRA standards and the regulations in most states, or they must produce them. Most attorneys do not do this. However, taking these few extra steps allows the practitioner to then obtain copies of such ADL flow sheets – often only facilitated through aggressive motion practice. They then take the significant amount of time necessary to compare them to the picture painted of the same resident in the MDS (Minimal Data Set). The results can be both shocking and fruitful in demonstrating truth on the ground. Without this additional hard work, nursing homes can typically avoid accountability suffered by their residents when they falsify these records. Inconsistency in these records, including falsified records of the bedsore (pressure ulcer) prevention mattress in use, is one of the sure signs of nursing home abuse.
FALSE CHARTING IN THE MAR's and TAR's
One of the most prolific examples of falsified records in long-term care for both nursing homes and assisted living facilities are Medication Administration Records (MAR) and Treatment Administration Records (TAR). These records essentially look like a grid or a graph paper, comprising one of the most important elements of a resident's chart; that is the provision of essential medications and of treatments.
They are at the very epicenter of what is happening to residents in these facilities and arguably paint a more thorough picture than actual nursing progress notes.
While more thought goes into nursing notes when catastrophic injuries and/or death occur, strategies of defensiveness often fall by the wayside during the day-to-day completion of these records. In my practice, there have been countless occasions where charts have been provided without such records. Quite often, they are then doctored after litigation commences, in order to sanitize the record in an attempt to paint it in a better light than that which actually occurred.
As long-term care facility residents frequently are outside of the building, careful inspection of the periods of time when they are not in the facility is an important component of the review of MAR's and TAR's.
It is important to set up a grid, which not only establishes when the resident was not in the building, but also days and times when the resident might be receiving dialysis care. Further, the hospitalizations which occur during a nursing home stay, it is essential not just to figure out which days the resident was not in the building, but to also closely inspect admission times and discharge times at the hospital.
Once armed with this information, the careful review of the MARs and TARs should commence. A significant percentage of long-term care litigation reveals the administration of medications and of treatments when residents were not even in the building. I have also found records indicating both treatments and medications administered to residents after they have died.
Having exposed such issues to a jury at the time of trial, I can assure the reader that this is explosive. More importantly, it exposes the truth as to what the worst of the worst nursing homes will do to avoid accountability. It is a time-consuming and difficult process. It involves a review not only of the nursing home chart, but also of ancillary medical records, such as hospitalizations and day visits to the hospital. It also can involve testimony to family members.
Ultimately, unless information revealed in this review is utilized as a tool at the time of deposition, its use at the time of trial is not nearly as effective. Of the two approaches utilizing these records, it is usually more effective to actually not confront the witness with the glaring inconsistencies and falsifications in the chart, but instead to carefully question the witness relative to the importance of accurate charting, the necessity of continuity of care, and the fact that the chart was not simply a meaningless paper exercise, but instead it is an essential component in ensuring competent and compassionate provision of care to all residents. Then, deposition testimony can also be utilized to elicit concessions from various staff members as to the penalties within the very home being litigated against as to penalties for falsification in a medical chart.
To be clear, there are no shortcuts here. It is slow, laborious and frequently does not bear fruit. However, in the careful review of long-term care records, it is an all-too-often overlooked strategy to expose the truth of abuses to these defenseless residents.
ORDERING MULTIPLE COPIES OF LONG-TERM CARE CHARTS TO UNCOVER FALSIFICATIONS
For nearly two decades, I have advised attorneys as to the importance of obtaining multiple copies of the same chart. It is a slow and expensive process, but essential in litigating long-term care abuse cases. At the outset of litigation, defenses of these facilities are often at their lowest.
Typically, counsel will be approached even before the nurse home administrator recognizes that litigation is forthcoming. For this reason, I have advised attorneys, by way of articles, texts and live presentations that clients themselves should be instructed to obtain their own copy of the records. These clients should be advised as to the contents of the OBRA Regulations (Omnibus Budget Reconciliation Act of 1986 –> 42 CFR 1983 et al). The OBRA Regulations require nursing homes to make records available within 24 hours of the request and copies of the same chart to be provided within 48 hours.
Unfortunately, the teeth to this regulation are not particularly sharp. That is, I do not counsel litigators to make a significant issue after a few extra days. However, when such requests involve more substantial delays, it is often the result of a hasty sanitization of the record. In these instances, I advise attorneys to promptly move forward with the Department of Health, for whichever state the case arises.
There is a school of thought promoting pre-suit litigation on this issue. I have found that this strategy, while sometimes effective, typically emboldens and empowers the homes, once they retain counsel. The length of time that the litigation encompasses actually provides the nursing home with additional time to falsify such records.
They are also at that juncture under the advice of defense counsel with regard to what they might take the position they do not need to produce. On the contrary, it usually only takes one phone call from the Department of Health to get the chart up right away, as nursing home administrators loathe citations. The more serious of citations incurred by nursing homes often result in their termination. A simple letter to the state, outlining attempts made to obtain the chart, courtesy copy of the applicable OBRA Regulations and a request for an investigation into the actual misconduct that led to the need for this litigation usually does the trick. It forces the nursing home to release the record before the actual lawsuit.
Another ancillary benefit is that the state will often investigate not only the delayed provision of records, but the actual misdeeds that injured your client. The primary function of having a client order the chart is to obtain those records before the nursing home is in the full sanitization process. It is important to segregate this chart, along with all transmittal letters. These will become quite useful as the case proceeds forward.
Once the case enters the next level, I advise attorneys to then order their own copy of the chart pre-suit through a simple letter, which also cites the applicable OBRA Regulations. Attorney letters will often also utilize citation of the appropriate regulations from the state in which the litigation is being sued. As one would expect, the nursing home then again provides the record. Again, these records should be reserved and maintained, along with all of the appropriate transmittal letters, as this will also be important further down the road.
Finally, it is almost inevitable that once defense counsel becomes involved (even after the previous double provision of the chart), they will be asked to and will produce another copy of the entire chart. Whichever sections are missing should also be requested. This will often involve motions and a significant level of tenacity. At this juncture, it should be ensured that whatever chart is provided is in color.
At this juncture, counsel should be possessed of three different copies of the chart. Again, significant work arises. All three copies should be carefully compared, page by page. This is a slow process. However, it is critical of the evaluation of any long term care case. Throughout the course of my practice I have found countless instances of alteration of medical records from each of these three incarnations of chart production. Often, nursing notes which did not exist in the first batch of records will appear in the second or third. It will be of no surprise that such records are germane to the actual injury and paints a picture that places the facility in a much better light than their absence would have.
There are other instances where records are literally changed. These alterations are not found easily. Further, I advise attorneys not to rely on their experts. Instead, attorneys should review the chart for purposes of determining whether or not the staff members at the facility have falsified its contents. While many experts happen upon falsifications, it is not the purpose of their review. This is the job of the attorney.
One must carefully review all of the records, not only those portions that seem medically relevant, but those that are seemingly innocuous. Only by engaging in this process, as expensive and time-consuming as it may be, are multiple instances true falsifications are exposed. Sadly, this practice is not universally followed, thus generating countless instances where such facilities get away with these falsifications.
FALSE RENTAL PAYMENTS IN LONG TERM CARE
Some of the most overlooked documents in long-term care litigation are the licensure file and cost reports for these facilities. Licensure files and Cost Report are free to obtain - other than modest copy fees. They contain a significant quantity of helpful and illuminating information about the structure and business activities of these very profitable businesses.
To be clear, in one's travels, even the most modest looking nursing home, dilapidated in appearance and small in structure typically is a $10,000,000.00 to $20,000,000.00 per year enterprise. This is because every resident in a nursing home is a revenue generator in the eyes of these businesses, in the amount of $8,000.00 to $12,000.00 per month. These bills are paid through Medicare and Medicaid – i.e. tax payer money. They are incredible profit centers for the long-term care industry.
Each bed in the building is incredibly profitable – usually generating over $100,000 in gross revenue annually. The problem is that PEOPLE live in those beds. Thus, nursing home incentivize their staff to keep as many beds filled are as possible. Many facilities incentivize staff by providing bonuses, depending on the level of the "census" of the building. Further, a low census often results in termination. I have been taken countless dozens of depositions on this issue, and have universally found that the issue of census is much more important in the professional life of those administrators than the quality of care reflected in the Department of Health Surveys – at least as to means by which owners conduct their reviews of work product.
Once nursing homes have a certain level of census within the building, they work extremely hard at maximizing its profitability - based upon each of these income-streams. As I will be discussing in other articles, one strategy utilized is to characterize these individuals as requiring super high levels of services on the Minimum Data Set records. This informs the rate of reimbursement that they receive for the care of any particular resident. However, such records typically do not reflect the actual condition or services received from these residents.
An additional profit-based strategy utilized by an alarmingly growing quantity of nursing homes is the use of reported artificially boosted rental payments. It is an elaborate scheme, wherein the owners of the actual nursing home operation will typically own the building and land of that business, but do so under different names and in such a fashion that it is difficult to determine that they are in fact the same people who own the actual business.
Once this ownership scheme is established, the nursing home must accordingly pay rent to its landlords. In reality, the landlord and the lessee of the very same individuals. However, on paper they appear to be different in operating an arms-length transaction. Once this paradigm is constructed, the artificial landlord is capable of charging as much rent as they desire out of the proceeds that the nursing home receives from Medicare and Medicaid.
On paper, the nursing homes can complain outwardly that the money provided by Medicare and Medicaid simply is not enough to take care of these people within their facility, especially in light of the ever rising rental payments they must pay to stay in the building. In reality, they are simply paying themselves exorbitant rent.
Uncovering this scheme is not simple. It requires one to obtain information relevant to the value of the property on which the nursing home sits, along with that of the building. This information is available online and also through the local tax assessor’s office. Once this is completed, the review of the licensure file and cost reports commences.
Cost reports are also available through public records requests via state and/or federal regulations. A view of these will often reveal rental payments well in excess of that which the market would otherwise bear. In my practice I have encountered a number of facilities where the same person actually signs as lessor and lessee on the lease. Such documents are not easy to come by and much work is involved to obtain them. They can be obtained from licensure files at times and often require requests through discovery. However, such documents will often reveal annual rental payments that even exceed the total value of the building and property.
Stated differently, there are situations where a building and land might be worth $1,000,000.00, and at the same time is subject to $1,000,000.00 per year leases. This means that what the owners are essentially doing is robbing residents of the money that is otherwise earmarked for the provision of care instead of lining their pockets, paying off their building in 1 year and reaping exorbitant profits - while appearing to be running a bare-bones operation with little or no profit. All of this is intimately related to the provision of care, based upon the fact that nursing homes do not provide competent care if there is not enough money to sufficiently staff and operate the facility.
TAMPERING WITH REPORTED STAFFING
In the world of for profit long-term care facilities, staffing represents the single most challenging expenditure of funds. That is, of all expenditures in the realm of long-term care, more money is spent of staffing costs than any other aspect of the enterprise. This means that the worst of such facilities are incentivized to do what they can to simply get by with regard to state inspections.
Citations for short staffing are extremely rare for a number of reasons, the most disturbing of which is the fact that many facilities will falsify these records. I have suggested to attorneys across this country that a careful inspection of reported staffing now is a critical part of the analysis in long-term care litigation. These documents can often be found in the state licensure file and can also be obtained through discovery. They are often handwritten.
Though a time consuming process, attorneys can gather a sufficient number of ancillary documents to then inspect the veracity of the staffing records. Often, these records are wholly inconsistent with the truth on the ground. Because they are handwritten, one should immediately look to the trends and for cross-outs. In my practice, I have seen threes converted into eights and ones converted into sevens. It represents an unrealistic increase in the quantity of staffing. I have also seen a diminution in the quantity of individuals residing in the building with notable infirmities, such as bed sores.
Stated differently, the level of acuity by necessity warrants the needs of nursing homes with regard to the quantity and quality of staff. The higher the acuity, the more care that is needed. When crunching the numbers, nursing homes often determine that the level of acuity does not match the quantity of staff that was already provided. They then will go back to staffing records and do what they can to these records to falsify the acuity levels - to give the appearance that they were less severe at any given time period than had previously been written contemporaneously about the staffing records and, at the same time, increase the number of staff from what was potentially accurately reported to what would need to have been the case to sufficiently staff and provide care for the residents.
It is not enough to simply get licensure files. Instead, it is important to get all of the additional ancillary records to address veracity of these documents. Once possessed of the results of this review, I advise attorneys to then take the essential depositions typically of individuals who have been prepared to address medical and nursing issues specifically - and certainly not staffing issues.
The benefit of approaching the deposition from what will seem to defense counsel as quite distant in left field, is that the truth often emerges. Asking challenging questions for which the witness has not been prepared related to staffing levels and even what has happened to staffing work leaders will often eliminate and entire defenses. Nursing homes are legally obligated to provide a compassionate and effective level of care. They cannot do this unless there are enough competent nurses, nurse's aides and other staff members in the building to accomplish this.
Exposing falsified staffing records allows the practitioner to dispute citations of the facility that they have provided sufficient staff to properly care for their vulnerable residents.
The Hidden Power of Requests for Admissions
The attached article was printed in the national publication, Trial. It highlights the incredible strength of Requests for Admissions as a litigation tool.
the_hidden_power_of_the_request_for_admissions-c (pdf)
DownloadOBRA
Published in the New Jersey Law Journal
Nursing Home Litigation - Fitting in the OBRA Regulations (pdf)
DownloadCorporate Shell Games
Published in the New Jersey Law Journal
The Nursing Home Shell Game - Holding Wrongdoers Accountable (pdf)
DownloadThe Role Of Physicians in Nursing Home Litigation
Published in the New Jersey Law Journal
The Role of Physicians in Nursing Homes - New Jersey Law Journa (pdf)
DownloadBedsores, Never Events and Nursing Home litigation
Published in the New Jersey Law Journal
Decubitus Ulcers (Bedsores) - NJ Law Journal (pdf)
DownloadManning the MInefield of Long term Care litigation
Cover story for the Estate Planning Supplement to the New Jersey Law Journal
Manning the Minefield of Long Term Care Regulations - New Jersey Law Journal (pdf)
DownloadTHOUGHTS ON LEGISLATION AFFECTING LONG TERM CARE LITIGATION
Injured Consumers and HR - 5 and HR 1215...Dangerous Legislation (pdf)
Download